What Exactly Is BHRT Anyway?

As a compounding pharmacist, I use the term “BHRT” all the time for describing hormone replacement therapy (HRT) for perimenopause and menopause. I find there is much confusion among patients and providers over BHRT (Bioidentical Hormone Replacement Therapy). BHRT refers to hormone replacement with ingredients that are “identical” to what your body produces.
Women make 3 estrogens…Estrone (E1), Estradiol (E2), and Estriol (E3), as well as Progesterone (P) and Testosterone (T). It makes sense to replace physiologic doses of identical hormones when levels drop and symptoms exist within scientific guidelines.
Small molecular changes make a big difference in how hormones work and fit into your receptors. Synthetic hormones are different chemical structures than endogenous human hormones. For example:
- Conjugated estrogens from horse urine (like what is found in the drug Premarin) are not the same as estrogens made by your body.
- ProgestINS like medroxyprogesterone acetate (sold under the brand name Provera among others), are not equal to progesterONE. We need Progesterone to maintain pregnancy, but medroxyprogesterone acetate is actually contraindicated during pregnancy.
- Methyltestosterone is not equal to testosterone.
When looking at hormone studies, it is important to understand what specific hormone was used, what dosing form, as well as the route of administration.
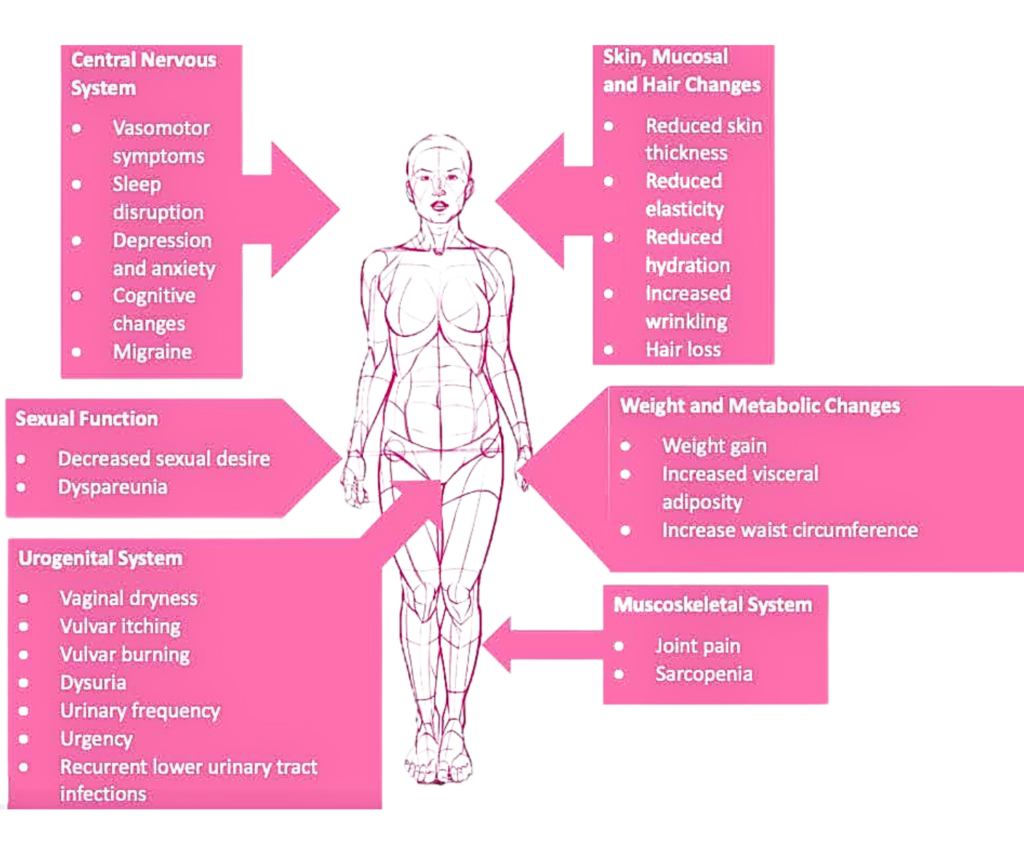
Symptoms Of Menopause
Women live 30 to 40 years after menopause so it is vastly important to resolve these symptoms via hormone balance for longevity and quality of life.
Health Benefits of HRT
Replacing hormones are beneficial for your bones, heart, brain, genitourinary system, sleep, weight loss, and mental health. Consider these facts:
- On average, 1 in 2 women over 50 will break a bone due to osteoporosis. Low levels of circulating estrogen are associated with an increased risk of postmenopausal osteoporosis, so this is a clear area when BHRT can make a difference.
- NAMS (North American Menopause Society) concluded that hormone therapy is the most effective treatment for vasomotor symptoms (hot flashes and night sweats) and genitourinary symptoms (vaginal dryness, irritation, recurrent urinary tract infections) and has been shown to prevent bone loss and fracture.
- Progesterone also increases bone formation, improves sleep, treats vasomotor symptoms, and has beneficial cardiovascular effects.
- Before menopause, women have a lower risk of coronary heart disease than men of the same age, but after menopause this risk increases. Estrogen modulates vascular (blood vessel) tone and protects the vascular endothelium (the important inner lining of blood vessels). Its loss contributes to reduced nitric oxide production, oxidative stress, and vascular dysfunction. Numerous studies show that there is a 40 to 50% risk reduction in cardiovascular morbidity and mortality with hormone replacement therapy.
- Estrogens have been shown to increase the cerebral circulation in women after menopause which has been associated with an improvement in memory and increases performance on cognition tests.
- Progesterone regulates neuronal plasticity, reduces anxiety and depression, and maintains memory.
Timing Is Key!
The Women’s Health Initiative (WHI) of 2002 was a large, long-term national health study that focused on preventing heart disease, cancer, and osteoporosis in postmenopausal women. The WHI as well as the Early Versus Late Intervention Trial with Estradiol (ELITE) showed that starting HRT within 5 to 10 years of menopause is fundamental to the success of estrogen’s cardioprotection in post menopausal women without adverse effects.
What About Breast Cancer?
The WHI’s estrogen-only arm showed a 28% decrease in Breast Cancer. Studies also show that Progesterone does not stimulate breast cells (unlike synthetic progestins). And significant evidence suggests no increased breast cancer risk with the use of testosterone.
NAMS (North American Menopause Society) states that the use of hormone therapy does NOT alter the risk for breast cancer in patients who have the risk factor of a family history of breast cancer. Those patients with risk factors can consider urine testing to study whether they are fully detoxifying their hormones as some estrogen by-products (metabolites) can be carcinogenic if they don’t break down properly. Additionally, patients can take supplements like DIM to support their hormone metabolism and detoxification systems.
Route Of Administration
The risks of hormone therapy differ depending on the type, dose, duration of use, route of administration, timing on initiation, and whether progesterone is used. Oral but NOT transdermal (cream or patch) estrogen replacement therapy is associated with increased risk of VTE (venous thromboembolism, or, blood clots in the veins). The transdermal route avoids the hepatic first-pass metabolism resulting in few adverse effects on coagulation markers (D-dimer, fibrinogen) compared to oral estrogens and does not increase the risk of DVT (deep vein thrombosis). Additionally, oral estrogen is associated with a marked and rapid increase in CRP (c-reactive protein), a marker for inflammation, whereas transdermal estradiol treatment is not. Oral estrogen also increases SHBG (sex hormone binding globulin) which decreases testosterone as well as growth hormone.
Why Choose Compounded BHRT?
Replacing hormones is not a one-size-fits-all approach. There are commercially available bioidentical medications, such as progesterone capsules and estradiol tablets, patches, gels, and vaginal creams. However, patients may need a different dose than what is available, or be allergic to an inactive ingredient such as the peanut oil in progesterone capsules, the adhesive on patches, the fillers in estradiol tablets, or the parabens in vaginal creams. Additionally, patients may need a different dosing form such as a transdermal cream which isn’t available commercially. Compounded BHRT offers many advantages in that we can customize treatment to each individualized patient.
Additionally, off-the-shelf options are not always available. For example, there is no commercially available testosterone prescription product for women, and the ones approved for men are not appropriate for use in women. Women with low testosterone often experience fatigue, brain fog, low mood, low libido, and exercise intolerance. There is also no commercially available form of estriol. Estriol can protect breast tissue (by occupying estrogen receptor sites on breast cells prohibiting E1 from binding), restores proper pH in the vaginal tract resulting in less UTI’s, and promotes a favorable environment for growth of lactobacilli (a “good bacteria” probiotic found in the human gut, mouth, and vagina).
What’s even better about BHRT? We can simplify your life by combining hormones into one dosing form. For example, once the proper dosing is tested and ascertained for any given patient, we could combine the E3/E2 and testosterone into one cream.The ideal method is to start with a low dosage and slowly increase for optimization and symptom resolution. Treatment should be personalized using the best available evidence to maximize benefits and minimize risks, then reevaluated every 6 to 12 months with a collaborative, shared decision making approach.
Hormone Consultations
A lot of providers reach out to us to say that they want to be able to offer hormone therapy to their patients, but they don’t have the time to devote to becoming a specialist on interpreting saliva tests and figuring out which dosage form to prescribe and at what ratio. On the flip side, we also have patients reach out to tell us that their doctor is on board for them starting hormone therapy and would happily prescribe it, they just need to know what to prescribe. We can help with both of these scenarios!
We are now offering women’s hormone therapy consultations in the form of a telehealth appointment, booked with me, where I will take a deep dive into your symptoms and medical history, interpret your labs, and give a recommended course of therapy for your provider to review and for you to discuss with your provider. Click here to book a hormone consultation appointment and enjoy $25 off appointments booked for May 2023!
If you have comments and/or questions about this blog, email us at blog@peoplesrx.com.

Deborah Fernandes is the Lead Compounding Pharmacist at Peoples Compounding Center and an HRT Specialist who has seen countless patients’ lives change for the better through compounded medications. To book an appointment for a private consultation with Deborah, click here.
REFERENCES:
Levin, V., et al. “Estrogen therapy for osteoporosis in the modern era,” Osteoporos Int 2018; 29(5):1049-55.
Prior, J., Progesterone for symptomatic perimenopause treatment—Progesterone politics, physiology and potential for perimenopause,” Facts Views Vis Obgyn 2011; 3 (2): 109-20.
Prior, J., “Progesterone for the prevention and treatment of osteoporosis in women,” Climacteric 2018; 21(4):366-74.
Naftolin, F.,et al., “Cardiovascular health and the menopausal woman: the role of estrogen and when to begin and end hormone treatment,” F1000 Res 2019, PMD31543950.
Gersh FL, O’Keefe JH, Lavie CJ
Postmenopausal hormone therapy for cardiovascular health: the evolving data Heart 2021;107:1115-1122.
Saleh, R., et al., “Hormone replacement therapy is associated with improved cognition and larger brain volumes in at-risk APOE4 women: results from the European Prevention of Alzheimer’s Disease (EPAD) cohort,” Alz Res Ther 2023; 15(1):10.
Theis, V. and Theiss, C. (2019), Progesterone Effects in the Nervous System. Anat Rec, 302: 1276-1286. doi:10.1002/ar.24121
The Women’s Health Initiative Steering Committee. Effects of Conjugated Equine Estrogen in Postmenopausal Women with Hysterectomy: The Women’s Health Initiative Randomized, Controlled Trial. JAMA. 2004; 291:1701-1712
Scarabin, P. Y., Oger, E., & Plu-Bureau, G. (2003). Differential association of oral and transdermal oestrogen-replacement therapy with venous thromboembolism risk. Lancet, 362(9382), 428–432. https://doi.org/10.1016/S0140-6736(03)14066-4
Mikkola, T. S., Savolainen-Peltonen, H., Venetkoski, M., & Ylikorkala, O. (2017). New evidence for cardiac benefit of postmenopausal hormone therapy. Climacteric, 20(1), 5–10. https://doi.org/10.1080/13697137.2016.1262839
Eilertsen AL, et al. The effects of oral and transdermal hormone replacement therapy on C-reactive protein levels and other inflammatory markers in women with high risk of thrombosis. Maturitas. 2005 Oct 16;52(2):111-8. doi: 10.1016/j.maturitas.2005.01.004. PMID: 16186073.
The NAMS 2017 Hormone Therapy Position Statement Advisory Panel. (2017). The 2017 hormone therapy position statement of The North American Menopause Society. Menopause, 24(7), 728–753.
https://doi.org/10.1097/GME.0000000000000921
